Future of Anesthesiology
Through disruptive re-birth, the field of anesthesiology will revolutionize medicine. The disruption is at the backbone of anesthesiology.
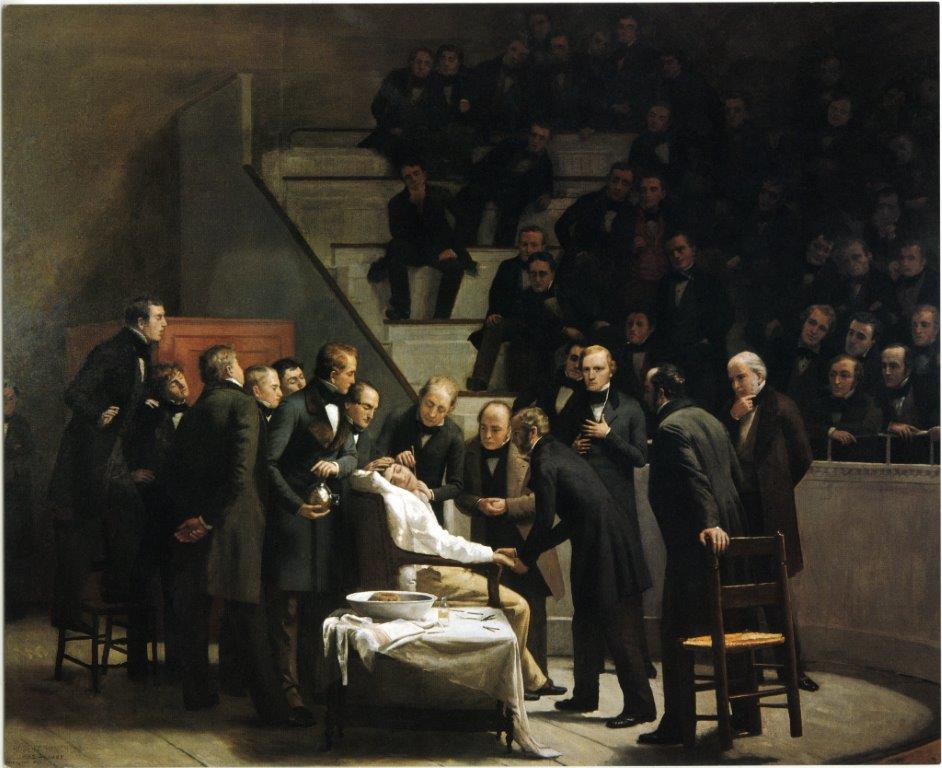
The first successful case of ether anesthesia performed by Dr. Morton at Massachusetts General Hospital in 1946 is an excellent example of a disruptive innovation that transformed and enabled the rapid development of many fields of medicine, drastically improving patient safety. The term disruptive innovation was first introduced by Clayton Christensen in 1997, referring to it as a process “by which a product or service takes root initially in simple applications at the bottom of a market and then relentlessly moves
We are uniquely positioned for the future. Anesthesia is a high-stakes and decision-intensive process-oriented discipline with continuous changes. New problems need to be quickly identified in the perioperative environment, and creative solutions within established best practices need to be thought of within very tight timing and resource constraints. These variable features make the field of anesthesiology ripe for innovation. The ubiquitous presence of technology, combined with a central position in hospital workflows, naturally exposes anesthesiologists to the cutting edge of medicine, engineering, and process management. A fluency in innovation is an increasingly valued skill in anesthesia. The role of the anesthesiologist in medicine uniquely positions the physician to observe, engineer, and influence processes in all aspects of healthcare delivery.

There are numerous areas of innovation in anesthesia, including workflow improvements, development of new devices, and the adoption of data science. The innovation of workflows utilizing novel techniques is perhaps a most underappreciated area for anesthesia. Phone applications and telemedicine allow for adequate supervision of patients in the operating room or intensive care unit. Several novel workflows have been identified in pain management, as well. We have seen innovation in device and process automation that allows closing the loop on parameter feedback, through continuous monitoring, adjustment of anesthesia levels, and personalization of responses to surgical stimulus. This additional intelligence infused into the workflow can help improve safety and outcomes. Science will enable anesthesiologists to influ

Peri-operative home vs. HOLISTIC care for surgery candidates.
More and more evidence suggests that pre-operative status is the most important determinant of recovery. Muscle mass, cardio-pulmonary endurance, or serum level of albumin are the most significant determinant of health. The cognitive function post-surgery depends on the pre-surgical performance of brain I, the memory, cognition, and other higher functions. Currently, peri-operative care is relegated to the optimization of drugs, “surgical clearance,” or some testing. This is obsolete and with little value. Anesthesiologists of the future will look at the patient as a project that requires several specialists needed for the optimization of the outcomes. This is a very different paradigm than the one practice in particular in the USA. It requires skill from the internal medicine area, physiotherapy, and nutrition. Planning of anesthesia will include the effect of different types of anesthesia and peri-operative environment on the short-term and long-term outcomes. Perhaps soon, we will know how anesthesia can modulate the recurrence of cancer or affect endothelial function. Anesthesia plan will be a tailor with these variables in mind. Delivery of anesthesia will be relegated to other providers. Anesthesiology is the line of defense for several cases sitting in the central command and supervising several patients remotely but close enough for direct intervention. AI and decision making processes will aid his/her task. Recovery will extend pass beyond 48hours. Ample evidence suggests that surgery can cause the emergence of new allosteric balance. This balance may have a detrimental effect on cognition, atherosclerosis, or another aspect of the nervous and immune system. It may be our domain to bring the patient to the optimal state as the surgery didn’t happen –  relegated to other providers. Anesthesiology is the line of defense for several cases sitting in the central command and supervising several patients remotely but close enough for direct intervention. AI and decision making processes will aid his/her task. Recovery will extend pass beyond 48hours. Ample evidence suggests that surgery can cause the emergence of new allosteric balance. This balance may have a detrimental effect on cognition, atherosclerosis, or another aspect of the nervous and immune system. It may be our domain to bring the patient to the optimal state as the surgery didn’t happen –
relegated to other providers. Anesthesiology is the line of defense for several cases sitting in the central command and supervising several patients remotely but close enough for direct intervention. AI and decision making processes will aid his/her task. Recovery will extend pass beyond 48hours. Ample evidence suggests that surgery can cause the emergence of new allosteric balance. This balance may have a detrimental effect on cognition, atherosclerosis, or another aspect of the nervous and immune system. It may be our domain to bring the patient to the optimal state as the surgery didn’t happen –
There is a case being made for the widespread adoption of data science, continuous sensors, genomics, and cloud computing. These will allow for ubiquitous machine learning and artificial intelligence use cases in anesthesia. This area of innovation offers the most transformative opportunities to impact the perioperative environment and the overall health care experience for both specialists and patients. New scenarios enabled by these technologies will emerge, where anesthesia can expand its current perioperative role and be involved earlier in the patient journey—covering the intraoperative experience, the ICU, and the home-based discharge process. The anesthesiologist’s leadership and participation in this expanded continuum of care can allow for a change in paradigm towards a personalized and continuous multi-factorial optimization of a surgical patient, improving surgical outcomes, survival, and safety not in perspective days but in months.

[1] Bowler, J.L., Christensen C.M., Disruptive Technologies: Catching the Wave. Harvard Business Review (1995).
[2] Kain, Z., Hwang, J. and Warner, M. Disruptive Innovation and the Specialty of Anesthesiology: The Case for the Perioperative Surgical Home. Anesthesia & Analgesia. (2015);120:5, p 1155-1157.
Special thanks to Gabriela Sabate @gsabate and Blair Clark-Schoen to contributing to this article